I have fantastic news -- I can continue to be your cardiologist!
Many of you whom I've spoken with have asked if I can continue to be your cardiologist. My answer was that I was in the process of contracting and to call me in January, because I was hopeful that I could continue to be your cardiologist, but I could not make that promise.
In the meantime, I have signed a contract with Regal and Lakeside for my new solo practice. If you are a Regal or Lakeside patient who has been seeing me, I can continue to be your cardiologist. However, please make sure that you request a new referral.
My staff and I are busy getting the office ready to open on January 2. Open house on Thursday January 25, 5:30-7:30 pm. More on that soon!!!
Saturday, December 23, 2017
Tuesday, December 05, 2017
To My Patients:
As you've heard, I'm leaving the position that I've held at Lakeside Community Healthcare for the past nine years, and I am starting my own cardiology practice.
I'll be opening up my office in Tarzana on January 2. It's a terrific location in the Safari Walk block of Ventura Boulevard, one half of a mile west of Tarzana Hospital. Another fantastic bonus of my location -- free parking!
I love my patients, and don't want to lose any of you. Some of us have known each other for nearly a decade.
You'll have the chance to come see my office on January 25, from 5:30-7:30 pm, when I'll have an open house for patients.
If you want to continue to have me as your cardiologist, please call my office in January at 818-938-9505. I am in the process of credentialing, so I do not know at the current time which insurers I will be able to accept, but I should know more soon.
And, if you're my current patient, and you want to see me in the office this month, call my Lakeside Burbank office at 818-848-0023.
I'll be opening up my office in Tarzana on January 2. It's a terrific location in the Safari Walk block of Ventura Boulevard, one half of a mile west of Tarzana Hospital. Another fantastic bonus of my location -- free parking!
I love my patients, and don't want to lose any of you. Some of us have known each other for nearly a decade.
You'll have the chance to come see my office on January 25, from 5:30-7:30 pm, when I'll have an open house for patients.
If you want to continue to have me as your cardiologist, please call my office in January at 818-938-9505. I am in the process of credentialing, so I do not know at the current time which insurers I will be able to accept, but I should know more soon.
And, if you're my current patient, and you want to see me in the office this month, call my Lakeside Burbank office at 818-848-0023.
Wednesday, November 08, 2017
New Practice Update!
It's been a lot of hard work, and there's just under two months until my new practice is open for business, January 2, 2018.
I have secured a fantastic location -- the Wall Street Building in Tarzana, Kravings restaurant is on the first floor, and there's a large Whole Foods Market across the street.
Now, I'm focused on the many details of my new medical practice. There's more to this than I had imagined -- credentialing with insurers, setting up wifi, computers, and phones, choosing an electronic medical record, hiring employees, buying equipment and furniture -- these are just a few of the tasks that I've had to take on.
But for me, the hardest part has been having to tell my patients that I'm leaving. I know some will follow me, and I'm so grateful for that, but others cannot, whether it be distance from home, or insurance. I've been with some of my patients for nearly nine years, and those office visits feel like meetings with old friends.
Stay tuned here for more details about my new practice!!
I have secured a fantastic location -- the Wall Street Building in Tarzana, Kravings restaurant is on the first floor, and there's a large Whole Foods Market across the street.
18663 Ventura Blvd, Tarzana
Now, I'm focused on the many details of my new medical practice. There's more to this than I had imagined -- credentialing with insurers, setting up wifi, computers, and phones, choosing an electronic medical record, hiring employees, buying equipment and furniture -- these are just a few of the tasks that I've had to take on.
But for me, the hardest part has been having to tell my patients that I'm leaving. I know some will follow me, and I'm so grateful for that, but others cannot, whether it be distance from home, or insurance. I've been with some of my patients for nearly nine years, and those office visits feel like meetings with old friends.
Stay tuned here for more details about my new practice!!
Thursday, October 05, 2017
Big News!!!
I am starting my own cardiology practice!
I've enjoyed my time working for Lakeside, and have appreciated my cardiology colleagues that I have had the honor to work alongside.
In my new practice, I look forward to providing a whole-person approach to cardiology. As someone who believes in the power of us as the drivers of our own health, my vision is a practice that encourages not just conventional medicine, but also lifestyle -- plant-powered food choices and movement to keep our hearts healthy.
Not only will I be able to provide top-notch cardiac care, but there will be plenty of additional enrichment opportunities. From nutrition seminars and individual consultations, to cooking classes and weight loss, this will be a full-service practice to help patients achieve optimal heart health.
Not only will I be able to provide top-notch cardiac care, but there will be plenty of additional enrichment opportunities. From nutrition seminars and individual consultations, to cooking classes and weight loss, this will be a full-service practice to help patients achieve optimal heart health.
Stay tuned..... once available, I will post my address here. Tentative office location is on the Safari Walk strip of Ventura Boulevard in Tarzana.
Sunday, October 01, 2017
International Plant-Based Nutrition Healthcare Conference
This year was my first visit to the International Plant-Based Nutrition Healthcare Conference in Anaheim, a massive 900+ gathering of doctors, nurses, health coaches, nutritionists and all sorts of healthcare providers assembled to learn about plant-based nutrition.
I arrived a day early to attend a seminar on how to market your plant-based medical practice, which will be very important (more on that topic soon!!). The next two and a half days were full of lectures from various doctors, nutritionists, and even a cooking demonstration!
This is what a full lecture hall looked like on the last day of the conference:
This was from Brenda Davis RD's talk. She gave an overview on the benefits of plant-based diets. Since I hear all day from patients telling me how they feel they need more protein, and personal trainers who push protein on their clients, I found this slide and the discussion around it very important:
Bottom line -- higher protein intakes, greater than 20% of calories per day, particularly when from animal sources, associated with increased mortality. That said, I would be cautious even with vegan protein supplementation.
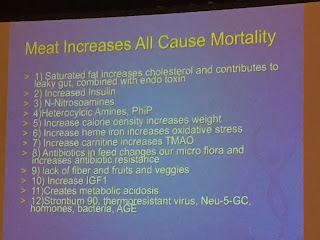
I clicked this slide from Dr. Garth Davis's talk. He and Dr. Kim Williams, the past president of the American College of Cardiology, gave exceptional talks. Dr. Davis put this slide up to summarize the ways meat increases mortality:
More reason to give up meat if you want to be healthy.
I think I nabbed this slide from Dr. Davis's talk as well. There's lots of people who are "pescevegan". They're vegan except that they do eat fish. (Ironically, I gave up fish at age 11 due to having fish for pets, but spent the next five years eating chickens and hamburgers and thinking nothing of it).
TMAO (trimethylamine-N-oxide) is found in the gut, and higher amounts are associated with increased plaque in the arteries. Fish consumption leads to the highest levels of TMAO. So, if one is concerned about health, here's another reason not to eat fish.
And of course, one of the coolest things about attending a course on plant-based nutrition -- the food!!!! Everything served was vegan, plant-based, and relatively healthy, either with no oil or minimal oil, minimal salt and sugar. I ate quite well.
I arrived a day early to attend a seminar on how to market your plant-based medical practice, which will be very important (more on that topic soon!!). The next two and a half days were full of lectures from various doctors, nutritionists, and even a cooking demonstration!
This is what a full lecture hall looked like on the last day of the conference:
This was from Brenda Davis RD's talk. She gave an overview on the benefits of plant-based diets. Since I hear all day from patients telling me how they feel they need more protein, and personal trainers who push protein on their clients, I found this slide and the discussion around it very important:
Bottom line -- higher protein intakes, greater than 20% of calories per day, particularly when from animal sources, associated with increased mortality. That said, I would be cautious even with vegan protein supplementation.
I clicked this slide from Dr. Garth Davis's talk. He and Dr. Kim Williams, the past president of the American College of Cardiology, gave exceptional talks. Dr. Davis put this slide up to summarize the ways meat increases mortality:
More reason to give up meat if you want to be healthy.
I think I nabbed this slide from Dr. Davis's talk as well. There's lots of people who are "pescevegan". They're vegan except that they do eat fish. (Ironically, I gave up fish at age 11 due to having fish for pets, but spent the next five years eating chickens and hamburgers and thinking nothing of it).
TMAO (trimethylamine-N-oxide) is found in the gut, and higher amounts are associated with increased plaque in the arteries. Fish consumption leads to the highest levels of TMAO. So, if one is concerned about health, here's another reason not to eat fish.
And of course, one of the coolest things about attending a course on plant-based nutrition -- the food!!!! Everything served was vegan, plant-based, and relatively healthy, either with no oil or minimal oil, minimal salt and sugar. I ate quite well.
Sunday, September 24, 2017
Busy times....
I haven't posted in a little bit. It's been a busy several weeks, as I study for my interventional cardiology board recertification exam on October 3.
I am attending the International Plant-Based Nutrition Healthcare Conference in Anaheim. Will share more on that later this week.
And, in sad news, I lost my dear greyhound Curves this week very suddenly. She would have been 12 in November. I had her in my life since September 2010. She loved to lie around, lying in the sun, playing with toys, and even fetching a ball. It's been hard, I can just be glad she didn't suffer long.
I am attending the International Plant-Based Nutrition Healthcare Conference in Anaheim. Will share more on that later this week.
And, in sad news, I lost my dear greyhound Curves this week very suddenly. She would have been 12 in November. I had her in my life since September 2010. She loved to lie around, lying in the sun, playing with toys, and even fetching a ball. It's been hard, I can just be glad she didn't suffer long.
Curves. 11/11/2005-9/22/2017
Sunday, July 30, 2017
Talking About Obesity
Talking to patients about weight isn't easy.
There's no question that obesity is a growing problem, with about a third of the population obese, and another third overweight.
But, just about no other condition lends itself more to ridicule and discrimination in our society. And yet no one wants to be obese; unfortunately, those eating and lifestyle habits that many consider "normal" lead to excess weight. Fat shaming is ever-present, and there's even research suggesting that people skip going to the doctor so that they can lose weight before their appointments.
So, how do I as a doctor discuss obesity with my patients? It's challenging. I want to help my patients without making them feel like they are being shamed; I want to be empathetic, but I do want to encourage changes that will lead to weight loss.
Regardless of my patient's body size, I ask the same questions of all new patients -- do you exercise? If not, why not? Tell me about your eating habits. Do you eat fruits and vegetables? Do you eat your meals at home? Do you do the grocery shopping? Do you know how to cook?
In someone who is obese, there are more likely to be answers to those questions that are less than ideal. And, as we talk, we discuss ways of making changes that will improve health and ultimately lead to weight loss.
Of my follow-up patients, I keep track of trends -- if an overweight patient is losing weight, we discuss how he is doing it. If a patient is gaining weight, I discuss with her what factors might be causing weight gain and how we can turn this around.
As a cardiologist, so many diseases that I treat -- coronary disease, atrial fibrillation, hypertension, hyperlipidemia -- are related to lifestyle and body size. I have helped many of my patients to lose extra weight, and hope to continue to do so.
There's no question that obesity is a growing problem, with about a third of the population obese, and another third overweight.
But, just about no other condition lends itself more to ridicule and discrimination in our society. And yet no one wants to be obese; unfortunately, those eating and lifestyle habits that many consider "normal" lead to excess weight. Fat shaming is ever-present, and there's even research suggesting that people skip going to the doctor so that they can lose weight before their appointments.
So, how do I as a doctor discuss obesity with my patients? It's challenging. I want to help my patients without making them feel like they are being shamed; I want to be empathetic, but I do want to encourage changes that will lead to weight loss.
Regardless of my patient's body size, I ask the same questions of all new patients -- do you exercise? If not, why not? Tell me about your eating habits. Do you eat fruits and vegetables? Do you eat your meals at home? Do you do the grocery shopping? Do you know how to cook?
In someone who is obese, there are more likely to be answers to those questions that are less than ideal. And, as we talk, we discuss ways of making changes that will improve health and ultimately lead to weight loss.
Of my follow-up patients, I keep track of trends -- if an overweight patient is losing weight, we discuss how he is doing it. If a patient is gaining weight, I discuss with her what factors might be causing weight gain and how we can turn this around.
As a cardiologist, so many diseases that I treat -- coronary disease, atrial fibrillation, hypertension, hyperlipidemia -- are related to lifestyle and body size. I have helped many of my patients to lose extra weight, and hope to continue to do so.
Wednesday, June 28, 2017
This Meme Needs To Go Away
I've seen this meme, and have been tagged with it, more times than I can count.
I'd be happy to see it go away. Why?
--First off, it's arrogant. It makes us vegans look like a--holes.
--Most cardiologists at this point are aware that meat-filled diets are associated with increased risk of heart disease. So I can't imagine a cardiologist telling a patient to go eat more meat.
--The meme assumes that if you're a vegan that you won't ever have heart disease. Not true at all. Tell that to my vegan patient with rheumatic heart disease, a consequence of scarlet fever as a child.
--While a vegan diet does help load the dice in your favor, you are not immune to hypertension, diabetes, elevated cholesterol or obesity, all of which I have seen in patients who proclaim themselves vegan.
--Or what about the patient who sees the light after a heart attack and decides to go vegan? My patients who have gone vegan after a major cardiac event have done great, I haven't needed to put a stent in any of them, nor have any of them had another heart attack. But, they still need a cardiologist even if they're eating a diet that Esselstyn, Ornish, McDougall, Fuhrman, and the rest of the vegan gurus would laud.
Let's be civil and make this obnoxious meme disappear. And when you see it again, please don't tag me. Thanks.
I'd be happy to see it go away. Why?
--First off, it's arrogant. It makes us vegans look like a--holes.
--Most cardiologists at this point are aware that meat-filled diets are associated with increased risk of heart disease. So I can't imagine a cardiologist telling a patient to go eat more meat.
--The meme assumes that if you're a vegan that you won't ever have heart disease. Not true at all. Tell that to my vegan patient with rheumatic heart disease, a consequence of scarlet fever as a child.
--While a vegan diet does help load the dice in your favor, you are not immune to hypertension, diabetes, elevated cholesterol or obesity, all of which I have seen in patients who proclaim themselves vegan.
--Or what about the patient who sees the light after a heart attack and decides to go vegan? My patients who have gone vegan after a major cardiac event have done great, I haven't needed to put a stent in any of them, nor have any of them had another heart attack. But, they still need a cardiologist even if they're eating a diet that Esselstyn, Ornish, McDougall, Fuhrman, and the rest of the vegan gurus would laud.
Let's be civil and make this obnoxious meme disappear. And when you see it again, please don't tag me. Thanks.
Sunday, May 21, 2017
A Woman in Medicine in 2017
I finished medical school in 1999. My class was about 54% female. Currently the field of physicians is close to 50/50 men and women. However, fewer than 20% of cardiologists are women. And, just under 6% of interventional cardiologists, my subspecialty, are women.
When sitting at a meeting of cardiologists, I'm more taken aback when I look across the table to see another woman cardiologist, than I am to walk into a room of all male cardiologists.
I can't say that there is often overt discrimination. I can say, however, that the female physician experience within my field, and likely others in medicine as well, is different from what a man would experience.
Recently, I attended a session on a new piece of technology for coronary intervention. As usual, I sat in an audience of all male cardiologists. I listened intently, and asked a question of the presenter about the availability of the product at other local hospitals that I cover. On my way out the door, a company representative approached me and asked, "Are you a hospital marketing professional?", not thinking that I just might be, like everyone else in the room, another interventional cardiologist.
A couple years ago, I was in the cardiac catheterization laboratory preparing to scrub a case. There were two operating suites. One of my male colleagues was working in the other suite. A representative for a device company, interestingly a woman, was in the lab that morning to promote her company's stent. As I was preparing for the procedure, she walked past me, not saying a word, into the lab next door where the male cardiologist was scrubbed.
Did she blow past me not knowing I was the physician? Did she assume that since I am a woman that I must be a nurse or a tech? I'll never know. But, most representatives promoting products will go to the small effort to find out which doctors will be scrubbed in each lab, and then introduce herself to the doctors.
The differences in how male and female physicians are treated tend to be more subtle. The patient who, just meeting me, feels comfortable addressing me by my first name, who likely would refer to a male physician using the title "doctor". The patient who refers to me as "hon" or "sweetie", who I promptly, but politely, will correct. Or, the patient, who upon me walking into the room, in my white coat, heels, and a dress, remarks, "You don't look like a doctor," or "I was expecting someone different", perhaps from the patient who didn't notice my first name on his or her appointment card and expected a more grey-haired man to be their cardiologist.
Or, a typical hospital scene: A female physician, a male nurse, a male physical therapist, and a male nursing aide are all working at a nursing station. A patient family member walks up to the nursing station to request a glass of water, another pillow, or something else for the patient. Who does the family member walk up to? The female physician.
There are other subtle differences. I've observed that bad behavior from men is tolerated often when it should not be. I watched one male cardiologist walk into a cath lab and scream (yes scream) at the staff because a patient was not ready. After he walked out, I turned to one of the techs and asked, "You put up with that behavior?" "That's just how he is," she said. I've seen male physicians chastise medical assistants for the smallest of details being missed and get away with it. And yet, I've found that I've had to adjust my own fairly direct manner of communication so as not to make others around me feel intimidated.
That said, there are benefits to being a woman physician. Women tend to be better listeners, and patients tend to be more comfortable opening up to women about their problems. The more comfortable a patient is to share what is going on in his life, the better I can be as a doctor to help him.
Even as women are more prevalent among physicians, old stereotypes, whether conscious or subconscious, still persist.
When sitting at a meeting of cardiologists, I'm more taken aback when I look across the table to see another woman cardiologist, than I am to walk into a room of all male cardiologists.
I can't say that there is often overt discrimination. I can say, however, that the female physician experience within my field, and likely others in medicine as well, is different from what a man would experience.
Recently, I attended a session on a new piece of technology for coronary intervention. As usual, I sat in an audience of all male cardiologists. I listened intently, and asked a question of the presenter about the availability of the product at other local hospitals that I cover. On my way out the door, a company representative approached me and asked, "Are you a hospital marketing professional?", not thinking that I just might be, like everyone else in the room, another interventional cardiologist.
A couple years ago, I was in the cardiac catheterization laboratory preparing to scrub a case. There were two operating suites. One of my male colleagues was working in the other suite. A representative for a device company, interestingly a woman, was in the lab that morning to promote her company's stent. As I was preparing for the procedure, she walked past me, not saying a word, into the lab next door where the male cardiologist was scrubbed.
Did she blow past me not knowing I was the physician? Did she assume that since I am a woman that I must be a nurse or a tech? I'll never know. But, most representatives promoting products will go to the small effort to find out which doctors will be scrubbed in each lab, and then introduce herself to the doctors.
The differences in how male and female physicians are treated tend to be more subtle. The patient who, just meeting me, feels comfortable addressing me by my first name, who likely would refer to a male physician using the title "doctor". The patient who refers to me as "hon" or "sweetie", who I promptly, but politely, will correct. Or, the patient, who upon me walking into the room, in my white coat, heels, and a dress, remarks, "You don't look like a doctor," or "I was expecting someone different", perhaps from the patient who didn't notice my first name on his or her appointment card and expected a more grey-haired man to be their cardiologist.
Or, a typical hospital scene: A female physician, a male nurse, a male physical therapist, and a male nursing aide are all working at a nursing station. A patient family member walks up to the nursing station to request a glass of water, another pillow, or something else for the patient. Who does the family member walk up to? The female physician.
There are other subtle differences. I've observed that bad behavior from men is tolerated often when it should not be. I watched one male cardiologist walk into a cath lab and scream (yes scream) at the staff because a patient was not ready. After he walked out, I turned to one of the techs and asked, "You put up with that behavior?" "That's just how he is," she said. I've seen male physicians chastise medical assistants for the smallest of details being missed and get away with it. And yet, I've found that I've had to adjust my own fairly direct manner of communication so as not to make others around me feel intimidated.
That said, there are benefits to being a woman physician. Women tend to be better listeners, and patients tend to be more comfortable opening up to women about their problems. The more comfortable a patient is to share what is going on in his life, the better I can be as a doctor to help him.
Even as women are more prevalent among physicians, old stereotypes, whether conscious or subconscious, still persist.
Monday, April 24, 2017
Passover Seder 2017
I hosted my annual seder. Twelve years ago when I first went vegan, there were exactly two vegan passover cookbooks, and if you would enter "vegan passover" into a search engine, my blog would be one of the first entries to come up! But now, there's lot of options, lots of cookbooks, and plenty of great vegan recipes for Passover.
We started with matza ball soup from Nava Atlas, the best vegan matza ball recipe around because the matza balls taste good and don't fall apart in water as they do in some vegan recipes.
Dinner, buffet style
Gefilte 'Fish' -- Maybe some things just should never be veganized. I was never a big fan of gefilte fish even as an omnivore. These actually came out quite good and were polished off, I added about half a cup of whole wheat matzah meal to make these patties a little firmer.
Spinach, leek and potato matzo gratin - avocado and cashews make a perfect sauce for between the layers. Recipe suggests adding Daiya vegan cheese -- no need.
Squash and roasted potatoes
"Bloody" potatoes -- mashed potatoes with beets, and sweet potato, carrot, and apple kugel
Ratatouille -- from the Vegan Start Passover Cookbook
Salad with candied walnuts and dried cranberries
My Plate
Desserts -- Chocolate matzo loaf, chocolate chip cookies, brownies, and fruit
Happy Passover!!!
Sunday, April 09, 2017
Life After Ironman
It's fun to post about achieving success as an athlete. But what happens when all that training winds down?
I started in the sport of triathlon in 2005. With hard work and good coaches, I peaked from 2012-2015. I worked out twice a day most days, six days a week, long workouts on the weekend. And I achieved a lot of success -- look back on blog post after blog post about race after race. And, even though it was hard work, I loved it, the people I've met, the adrenaline rush of racing, great conversations on long bike rides and runs.
After Ironman Boulder 2015, for several reasons, a bit of burnout and some other personal stuff, I decided to take a step back from all the hard training. I certainly didn't become a couch potato, but what I do now is a far cry from back then.
And there are consequences of the decreased training load. Some are good -- I'm less stressed out because I don't have to worry about fitting in my workouts. I don't have to figure out how to do a four hour bike ride while remaining within twenty minutes of my car in case someone needs an emergency angioplasty. And, I have more time for things like sleep and weekend brunch.
But, I'm definitely not as fast, particularly as a runner. I found that out in a big way when I ran a half marathon in December, hoping for one goal and definitely not achieving it. And my body has changed. I'm not heavy, but I certainly don't look as ripped as I do in the photo from the frequently circulated article about me on Forks Over Knives.
There's guilt too -- I'm so used to doing morning and evening workouts, am I really exercising enough if I run in the morning and don't do anything else later? Or if I decide to sleep in past 5:30 am? And people still ask, "When's your next Ironman?" Am I still worthy of the reputation I've gained as the VeganHeartDoc who swims/bikes/runs like crazy?
I had a lot of reasons to tone down my training. I don't regret it. I still work out six days a week, but most of the time it's just one workout a day, not two. I'm training for a marathon at the end of May, the Mountains to Beach Marathon. Initially I thought my goal for the race would be 4:20, but I may be finishing in the high 4's. And that's ok.
I started in the sport of triathlon in 2005. With hard work and good coaches, I peaked from 2012-2015. I worked out twice a day most days, six days a week, long workouts on the weekend. And I achieved a lot of success -- look back on blog post after blog post about race after race. And, even though it was hard work, I loved it, the people I've met, the adrenaline rush of racing, great conversations on long bike rides and runs.
I earned all this good stuff
And there are consequences of the decreased training load. Some are good -- I'm less stressed out because I don't have to worry about fitting in my workouts. I don't have to figure out how to do a four hour bike ride while remaining within twenty minutes of my car in case someone needs an emergency angioplasty. And, I have more time for things like sleep and weekend brunch.
But, I'm definitely not as fast, particularly as a runner. I found that out in a big way when I ran a half marathon in December, hoping for one goal and definitely not achieving it. And my body has changed. I'm not heavy, but I certainly don't look as ripped as I do in the photo from the frequently circulated article about me on Forks Over Knives.
There's guilt too -- I'm so used to doing morning and evening workouts, am I really exercising enough if I run in the morning and don't do anything else later? Or if I decide to sleep in past 5:30 am? And people still ask, "When's your next Ironman?" Am I still worthy of the reputation I've gained as the VeganHeartDoc who swims/bikes/runs like crazy?
I had a lot of reasons to tone down my training. I don't regret it. I still work out six days a week, but most of the time it's just one workout a day, not two. I'm training for a marathon at the end of May, the Mountains to Beach Marathon. Initially I thought my goal for the race would be 4:20, but I may be finishing in the high 4's. And that's ok.
Sunday, February 12, 2017
Living alone -- not an excuse!!!
I hate excuses. It's always easier to find a reason not to make the right choice than it is to go to the effort to make healthy choices. Such as, when patients tell me they haven't exercised in a month because it's too hot, it's too cold, it rained.... it's Southern California, give me a break!
But, when it comes to making good food choices, I often hear from patients that they live alone, so it's too hard to shop for one, keep food from going bad, and take the time to prepare a meal. So, instead, they resort to fast food, restaurants and prepared meals, which nutritionally are poorer quality than most of what you might otherwise prepare in your kitchen.
I can debunk the living alone excuse quite easily, because for most of the past ten years, other than my adorable greyhound companions, I've lived alone. I prepare most of my meals at home, and it's not that hard to do.
Shopping
I buy much of my produce at the Sherman Oaks Farmers Market on Tuesday evenings. It's a stop on my way home from work. For other food, I'll usually shop once a week. I'll pick up the basics at Trader Joe's, because they offer good prices and plenty of organic options. I buy a few things in bulk at Costco like organic baby carrots, And, because I can walk down the street to Whole Foods, I pick up odds and ends from there.
Food Prep
Often, I'll spend a weekend morning, or an evening, preparing some staples, so that it's easier during the week.
I love my steaming baskets. I'll put them on top of a pan of simmering water, add vegetables, and cover with a lid to keep the steam in. Here I cut up some red peppers. After these cooked for about ten minutes, I then steamed some purple cabbage and baby carrots.
But, when it comes to making good food choices, I often hear from patients that they live alone, so it's too hard to shop for one, keep food from going bad, and take the time to prepare a meal. So, instead, they resort to fast food, restaurants and prepared meals, which nutritionally are poorer quality than most of what you might otherwise prepare in your kitchen.
I can debunk the living alone excuse quite easily, because for most of the past ten years, other than my adorable greyhound companions, I've lived alone. I prepare most of my meals at home, and it's not that hard to do.
Shopping
I buy much of my produce at the Sherman Oaks Farmers Market on Tuesday evenings. It's a stop on my way home from work. For other food, I'll usually shop once a week. I'll pick up the basics at Trader Joe's, because they offer good prices and plenty of organic options. I buy a few things in bulk at Costco like organic baby carrots, And, because I can walk down the street to Whole Foods, I pick up odds and ends from there.
Food Prep
Often, I'll spend a weekend morning, or an evening, preparing some staples, so that it's easier during the week.
I love my steaming baskets. I'll put them on top of a pan of simmering water, add vegetables, and cover with a lid to keep the steam in. Here I cut up some red peppers. After these cooked for about ten minutes, I then steamed some purple cabbage and baby carrots.
I like to have a grain on hand as well. Often it will be quinoa or brown rice, but today I decided on Trader Joe's Harvest Grains Blend with Israeli couscous.
I like to roast a few items in the oven as well. Today I roasted brussel sprouts in oil, Braggs Organic Sea Kelp Delight, and some sea salt. I put a couple of large Japanese sweet potatoes in the oven. And, I roasted a butternut squash, which I'm probably going to turn into a soup by spinning it in my Vitamix with some veggie broth.
After I finished cooking and chopping up some herbs and cucumbers, I put it all in the fridge.
What I Eat
I do not spend a long time preparing meals. I grab a few items from the fridge and usually put them in a bowl. I try to keep my meals half vegetable, one quarter grain, and one quarter protein (beans, lentils, cut up tofu, etc).
And, I may have the same thing a few days in a row, because honestly it's easier. For example, recently I bulk cooked quinoa. I put some in my salad for dinner, and the next morning, instead of making oatmeal, I put some quinoa in a bowl, added soy milk, frozen mango and berries, and chia seeds, and microwaved it for a delicious hot breakfast bowl.
Eating well when you live alone isn't that hard -- it just takes a bit of planning.
Sunday, January 08, 2017
Doctor Visit Pearls
From my point of view as a doctor, here are a few tips, some obvious and some not so obvious:
What's the quickest way to get in and out for your appointment? Book the first appointment of the day. I try my best to be on time, but it can be hard.
Are you a new patient with a complicated history, or have you had a number of tests done with a previous doctor? Bring in those records, especially if you received care out of town. We can always have you sign a release in the office, which means we will obtain the records after you leave, but it is so much easier to have the records at the initial consultation.
Know your medications. And their doses. If you are unsure of either, bring a list, or bring all the bottles.
Don't just stop your medications on your own without communicating to your doctor who prescribed the medicine. I've seen some absolutely catastrophic events occur when patients take it upon themselves to decide a medication is not needed -- stents clotting off, congestive heart failure, heart attacks, and strokes, to name just a few.
Skip the excuses. If you gained five pounds when you were supposed to lose weight, have been eating crap, and haven't exercised, don't tell me how you're busy and stressed out. We're all busy. And your heart doesn't care. There will always be excuses not to do the right things, and your bad habits will catch up with you and your health will suffer. Own up and make a plan to do better going forward to take care of yourself.
Use your appointment time wisely. Your doctor does have a limited amount of time, so be focused, Know why you came and get the answers that you need. You wouldn't ask a fisherman how to herd cattle, so don't ask me a question better suited for a different specialist.
Be nice to the office staff. The receptionists, medical assistants, and medical records workers are all critical to the function of any good office practice. They work hard and deserve respect. And, you can rest assured that your doctor will know if you were rude, even if you are saccharine-sweet in the exam room.
If you don't understand, ask. I love questions. It shows me that a patient is invested in their own health and is motivated. As doctors we are teachers, and I love to empower my patients to take control of their health.
After the visit, do not be afraid to communicate. You don't understand your instructions? The pharmacy didn't receive your prescription? You're having what could be a reaction to a medicine? Please call. Or, e-mail. My office has a secure email communication system. Your message goes straight to the doctor.
What's the quickest way to get in and out for your appointment? Book the first appointment of the day. I try my best to be on time, but it can be hard.
Are you a new patient with a complicated history, or have you had a number of tests done with a previous doctor? Bring in those records, especially if you received care out of town. We can always have you sign a release in the office, which means we will obtain the records after you leave, but it is so much easier to have the records at the initial consultation.
Know your medications. And their doses. If you are unsure of either, bring a list, or bring all the bottles.
Don't just stop your medications on your own without communicating to your doctor who prescribed the medicine. I've seen some absolutely catastrophic events occur when patients take it upon themselves to decide a medication is not needed -- stents clotting off, congestive heart failure, heart attacks, and strokes, to name just a few.
Skip the excuses. If you gained five pounds when you were supposed to lose weight, have been eating crap, and haven't exercised, don't tell me how you're busy and stressed out. We're all busy. And your heart doesn't care. There will always be excuses not to do the right things, and your bad habits will catch up with you and your health will suffer. Own up and make a plan to do better going forward to take care of yourself.
Use your appointment time wisely. Your doctor does have a limited amount of time, so be focused, Know why you came and get the answers that you need. You wouldn't ask a fisherman how to herd cattle, so don't ask me a question better suited for a different specialist.
Be nice to the office staff. The receptionists, medical assistants, and medical records workers are all critical to the function of any good office practice. They work hard and deserve respect. And, you can rest assured that your doctor will know if you were rude, even if you are saccharine-sweet in the exam room.
If you don't understand, ask. I love questions. It shows me that a patient is invested in their own health and is motivated. As doctors we are teachers, and I love to empower my patients to take control of their health.
After the visit, do not be afraid to communicate. You don't understand your instructions? The pharmacy didn't receive your prescription? You're having what could be a reaction to a medicine? Please call. Or, e-mail. My office has a secure email communication system. Your message goes straight to the doctor.
Subscribe to:
Comments (Atom)